Image: freepik.com
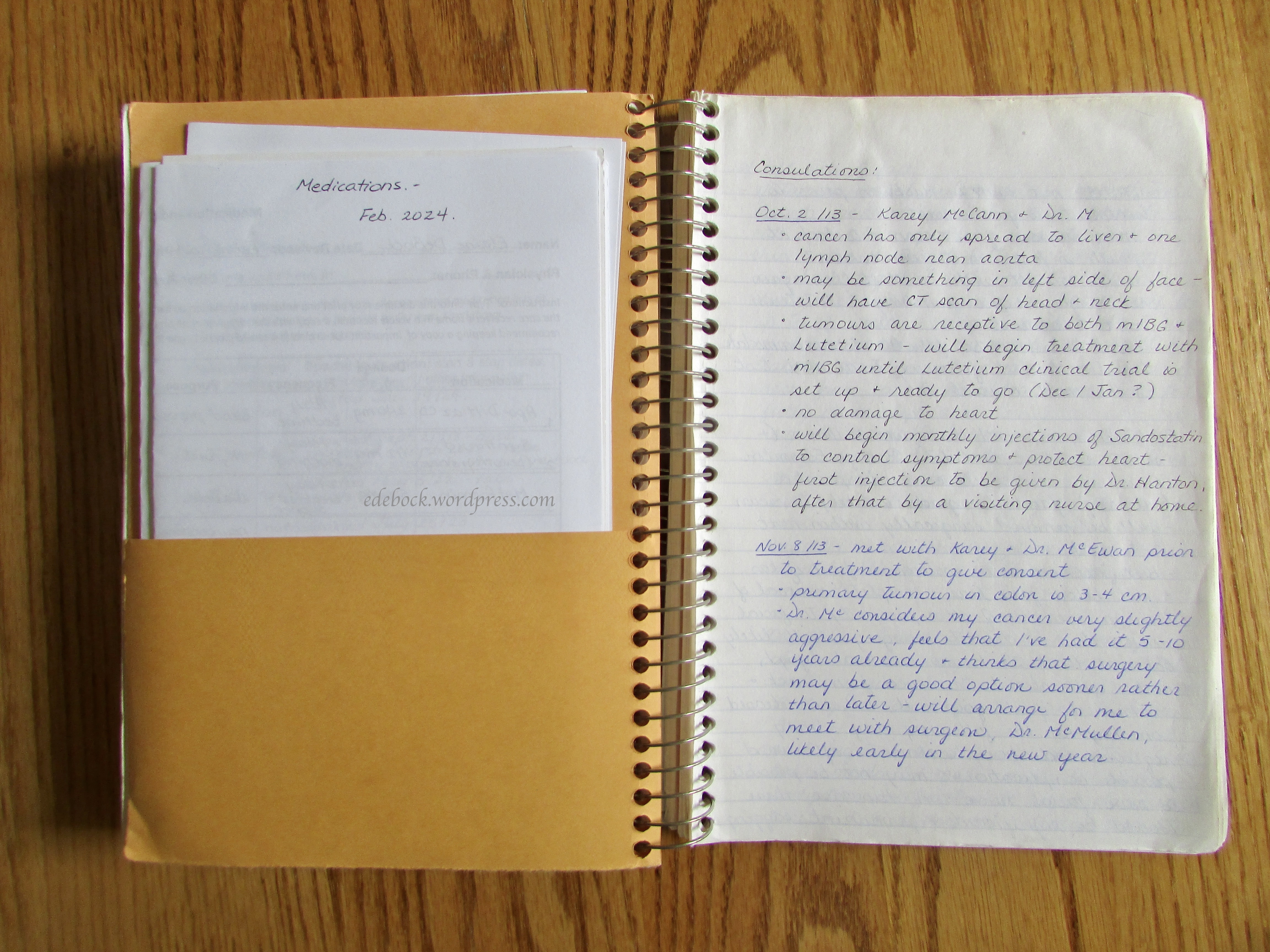
While most people mean well, knowing what to say to a cancer patient can be challenging and as a result, many people say things that are are far from helpful. As you know, I have chosen to be very transparent about my experience and how I’m doing. For the most part, people have been supportive and I appreciate that greatly, but I’ve also been taken aback by some of the things that have been said. So, from the perspective of someone who has been dealing with the disease for over a decade, here are 12 things not to say to someone with cancer.
I know how you feel.
No you don’t! Even if you have or have had cancer yourself, everyone experiences the journey uniquely. As similar as your story might be, how you felt might be completely different from how the person you’re speaking with feels.
My aunt / grandmother / next door neighbour’s cousin had cancer and they…
There are more than 200 different kinds of cancer and even two people with the same kind may experience it and its treatment entirely differently.
My friend / family member died of cancer.
It is never a good idea to remind someone who is battling cancer that people die of the disease. We already know that! We all know someone who died of cancer. We don’t need to be reminded of our mortality.
Do they know what caused it?
Saying this seems to imply that the person might have an underlying genetic flaw or worse, that unhealthy lifestyle choices might have led to their diagnosis. Many of us have no known risk factors or family history that would explain our cancers and introducing feelings of doubt or guilt are not helpful!
You should try [insert an alternative therapy here].
This is one of my pet peeves! It is never okay to suggest that a patient might not be getting the best care possible or that you, an armchair expert, know better than the professionals in the field of cancer care. The rule of thumb here should be, don’t give any advice unless you’re asked for it.
You should eat more / stop eating …
This is another one that really irks me. I’ve been given so much, and sometimes even conflicting, dietary advice by well-meaning people that I could probably write an entire blog post about it, but I won’t. Good nutrition is important during cancer treatment, but there is absolutely no scientific evidence that certain foods or specific diets can cure cancer.
Big pharma is blocking or withholding new cancer treatments.
This is one of many common myths or misconceptions about cancer treatment that should be stopped in its tracks. Unfortunately, scientific studies and clinical trials to determine the safety and effectiveness of new cancer treatments take time. That may create the appearance or lead to reports that effective new treatments are being blocked, but that simply isn’t the case. No one is hiding the cure to cancer or withholding help from those who need it.
A positive attitude is all you need to beat cancer.
There is absolutely no scientific proof that a positive attitude gives you an advantage in cancer treatment or improves your chance of survival. It does, however, improve your quality of life during cancer treatment and beyond. I can definitely attest to that, but it’s also a reality that no one can stay positive all the time. Everyone will have down days.
You don’t look sick. It must not be that bad. or You don’t look like you have cancer.
Outward appearance isn’t always indicative of how serious a person’s cancer is. I may look good on the outside, but you can’t see the mess that my insides are in!
You’re so brave.
No, I’m not! Courage is choosing to willingly confront agony, pain, danger, uncertainty, or intimidation. Those of us with cancer didn’t have any choice in this. We are simply dealing with what was dealt us and trying to make the best of a bad situation.
God won’t give you more than you can handle.
Oh, yes he will! Nowhere in scripture does it say that God won’t give us more than we can handle. In fact, it says that there will always be suffering, trials, temptations, pain, and situations that we won’t be able to handle on our own. It also promises that He will be with us through those times. We aren’t meant to handle them on our own; we’re meant to depend on Him.
Let me know if there’s anything I can do.
While this sounds great, it’s too vague. Instead, offer something more specific. Ask if they need a ride to appointments or if some freezer meals would be helpful after a treatment or surgery. If they have children, offer to provide childcare while they receive medical care or just take a much needed break. When you make a specific offer, the person can say yes or no, and they are also more likely to ask for help when they actually need it.
Several of these tips would also apply to other serious illnesses as well as to loss. Sometimes it’s better not to say anything at all than it is to say the wrong thing. In fact, your presence is often what’s needed most. Simply be there; be willing to listen if the person wants to talk, but understand if they don’t. Even those of us who are very open about what we’re going through want to be seen as more than just a person with cancer, so talk to us about the same things you’d talk to anyone else about.