As a neuroendocrine cancer (NETS) patient for the past ten years, stable became one of my favourite words. After each set of tests and scans, stable was the word that my doctors used to tell me that my cancer had not grown or spread. Unfortunately, when I saw my specialist on Friday, that was not what I heard. Instead, I heard the word progression.
In the cancer world, progression is the word that is used to describe growth or spread of the disease. It didn’t come as a shock to me. Over the past few months, we’ve been carefully watching test results that appeared to indicate that my tumours were likely becoming more active again. The news we heard on Friday was actually better than I feared. There has been a tiny bit of growth to a couple of tumours on my liver, but no spread anywhere else. That part is very good news!
Thankfully, I’m a cup half-full kind of person. I think I’d be a basket case by now if I wasn’t!

So, what’s the good news in this? What happens next and what’s there to be optimistic or hopeful about?
After 126 monthly injections of a drug called Sandostatin, it would appear that it’s no longer doing its job and I’ll be switching to a different medication. Since Lanreotide is also given as an injection every 28 days there will be little change to the routine that we’ve become accustomed to over the years. There are, however, some real benefits to this medication.
Unlike Sandostatin which is know to suppress the production of the hormones that these tumours produce and thus reduce symptoms, Lanreotide is also known to actually delay their growth. Secondly, Novartis, the company that produces Sandostatin, cut out their in-home injection program over a year ago and I had to arrange for my family doctor to begin giving me my injections. Lanreotide is produced by Ipsen and I’ve been assured that once again, a nurse will begin visiting my home to administer my butt jabs. Not only is that more convenient for me, but it frees up my doctor’s time for other patients which is an important issue in a rural area where there’s a doctor shortage. Perhaps the most exciting part of all this for me, if there can be excitement in receiving news of progression, is the fact that hubby and/or I can be taught to administer the Lanreotide injections ourselves! Why is that exciting, you ask? Why would I want to poke myself if a visiting nurse could do it for me? For someone who loves to travel, as I do, the idea that I might be able to pack my medication and leave the country for more than 28 days at a time is actually quite exhilarating!
I’m already somewhat familiar with the new drug because many people in my online patient groups are on it and seem to tolerate it well. Hopefully I will too. I’ll have tests and scans again in late October to see if it’s having the desired effect. In the meantime, it’s summer in Alberta. There’s camping, hiking, and kayaking to be done and golf to play. In spite of the change from stable to progression, I still feel 100% and I’m determined to keep on living life to the fullest.



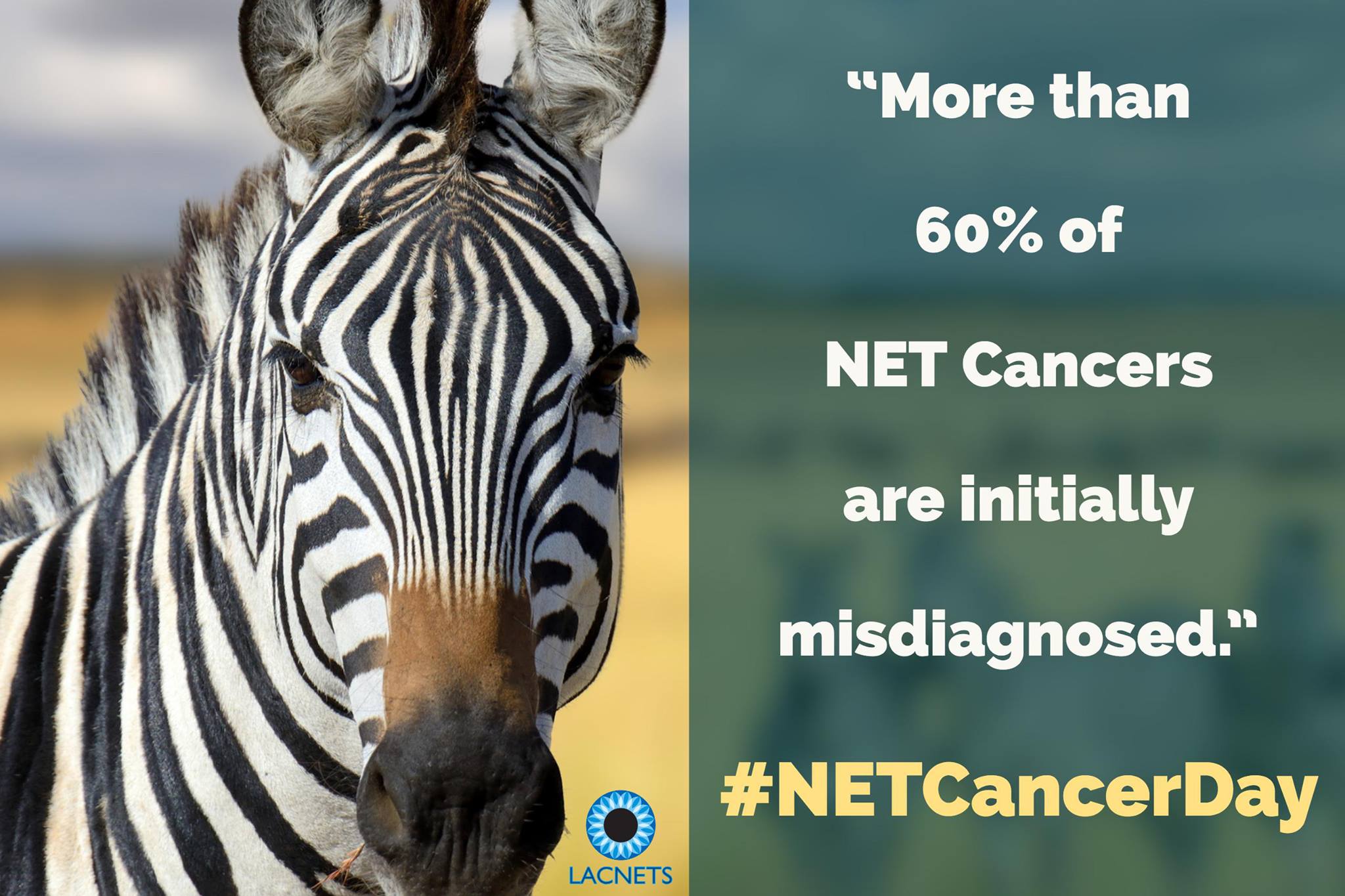
 Once again, today is Worldwide NET Cancer Day, a day set aside to increase awareness of neuroendocrine (NET) cancers and to promote improved diagnostics, treatments, information, care and research. As a patient who has been living with this cancer for the past nine years, this is, of course, very close to my heart.
Once again, today is Worldwide NET Cancer Day, a day set aside to increase awareness of neuroendocrine (NET) cancers and to promote improved diagnostics, treatments, information, care and research. As a patient who has been living with this cancer for the past nine years, this is, of course, very close to my heart.
 As always, the blog will be about more than cancer, but from time to time I will be using it to share progress reports. The only difference from the past will be that now I’ll be reporting on both of us!
As always, the blog will be about more than cancer, but from time to time I will be using it to share progress reports. The only difference from the past will be that now I’ll be reporting on both of us!